Karies gigi
| Karies gigi | |
|---|---|
 | |
| Kerusakan gigi berupa lubang yang disebabkan karies | |
| Informasi umum | |
| Spesialisasi | Kedokteran gigi |
Karies gigi adalah sebuah penyakit infeksi yang merusak struktur gigi.[1] Penyakit ini menyebabkan gigi berlubang. Jika tidak ditangani, penyakit ini dapat menyebabkan nyeri, penanggalan gigi, infeksi, berbagai kasus berbahaya, dan bahkan kematian. Penyakit ini telah dikenal sejak masa lalu, berbagai bukti telah menunjukkan bahwa penyakit ini telah dikenal sejak zaman Perunggu, zaman Besi, dan masa pertengahan.[2] Peningkatan prevalensi karies banyak dipengaruhi perubahan dari pola makan.[2][3] Kini, karies gigi telah menjadi penyakit yang tersebar di seluruh dunia.
Ada beberapa cara untuk mengelompokkan karies gigi.[4] Walaupun apa yang terlihat dapat berbedam faktor-faktor risiko dan perkembangan karies hampir serupa. Mula-mula, lokasi terjadinya karies dapat tampak seperti daerah berkapur namun berkembang menjad lubang coklat. Walaupun karies mungkin dapat saja dilihat dengan mata telanjang, terkadang diperlukan bantuan radiografi untuk mengamati daerah-daerah pada gigi dan menetapkan seberapa jauh penyakit itu merusak gigi.
Lubang gigi disebabkan oleh beberapa tipe dari bakteri penghasil asam yang dapat merusak karena reaksi fermentasi karbohidrat termasuk sukrosa, fruktosa, dan glukosa.[5][6][7] Asam yang diproduksi tersebut mempengaruhi mineral gigi sehingga menjadi sensitif pada pH rendah. Sebuah gigi akan mengalami demineralisasi dan remineralisasi. Ketika pH turun menjadi di bawah 5,5, proses demineralisasi menjadi lebih cepat dari remineralisasi. Hal ini menyebabkan lebih banyak mineral gigi yang luluh dan membuat lubang pada gigi.
Bergantung pada seberapa besarnya tingkat kerusakan gigi, sebuah perawatan dapat dilakukan. Perawatan dapat berupa penyembuahan gigi untuk mengembalukan bentuk, fungsi, dan estetika. Namun belum diketahui cara bagaimana untuk meregenerasi secara besar-besaran pada struktur gigi. Maka, organisasi kesehatan gigi terus menjalankan penyuluhan untuk mencegah kerusakan gigi, misalnya dengan menjaga kesehatan gigi dan makanan.[8]
Sejarah

Bukti arkeologis menunjukkan bahwa karies gigi sudah ada sejak masa prasejarah. Sebuah tengkorak yang diperkirakan berasal dari satu juta tahun yang lalu dari masa neolitikum memberi petunjuk adanya karies.[2] Adanya peningkatan prevalensi karies sejak masa neolitikum mungkin disebabkan banyaknya konsumsi makanan dari tumbuhan yang banyak mengandung karbohidrat.[9] Sebuah gurdi atau bor dari kayu ditemukan pada masa neolitikum. gurdi tersebut diperkirakan digunakan sebagai pelubang gigi untuk mengeluarkan abses dari gigi.[10] Perubahan kebudayaan berupa penemuan teknik pertanian di Asia Selatan dipercayai juga sebagai salah satu peningkat prevalensi karies.
Sebuah teks dari Sumeria (5000 SM) menggambarkan sebuah "cacing gigi" sebagai penyebab karies.[11] Bukti pada kepercayaan ini juga ditemukan pada India, Mesir, Jepang, dan Tiongkok.[3]
Banyak fosil tengkorak yang dapat menunjukkan adanya perawatan gigi yang primitif. Di Pakistan, sebuah gigi yang diperkirakan berasal dari 5500 SM hingga 7000 SM menunjukkan sebuah lubang yang mungkin disebabkan gurdi gigi. [12] Karies juga dituliskan oleh Homer dan Guy de Chauliac dalam tulisan mereka.[3] Papirus Ebers, sebuah tulisan Mesir kuno (1550 SM) menyebutkan sebuah penyakit gigi.[11] Selama pemerintahan dinasti Sargonid Assyria pada 668 SM hingga 626 SM, dituliskan bahwa dokter kerajaan memerlukan tindakan pencabutan gigi untuk mencegah penyebaran radang.[3] Selama masa pendudukan bangsa Romawi di Eropa, proses pemasakan makanan menurunkan tingkat terjadinya karies.[13] Pada masa peradaban Yunani dan Romawi dan Mesir, memiliki perawatan untuk meredakan rasa nyeri karena karies.[3]
Tingkat kejadian karies menurun pada masa Perungggu dan Besi, namun meningkat tajam pada masa pertengahan.[2] Peningkatan prevalensi karies secara periodik ini serupa dengan kejadi pada masa tahun 1000, ketika gula menjadi lebih mudah didapatkan di dunia Barat. Perawatan yang diberikan berupa obat-obatan herbal dan jampi-jampi, serta pencabutan gigi.[14][3]Umat Katolik menyampaikan doa dengan penyertaan Santo Appolonia, santo pelindung untuk dokter gigi.[15]
Ada pula bukti yang menunjukkan adanya peningkatan tingkat karies di suku Indian, Amerika Utara setelah memulai kontak dengan kolonial Eropa. Sebelum kolonisasi, Indian Amerika Utara menggantungkan hidupnya pada berburu, kemudian berubah menjadi bertani jagung. Pergantian diet makan ini menyebabkan peningkatan karies.[2]
Pada masa pencerahan, kepercayaan bahwa "cacing gigi" sebagai penyebab karies ditepis oleh kelompok ilmuwan kedokteran.[16] Pierre Fauchard, yang dikenal sebagai bapak kedokteran gigi masa kini, adalah salah satu pihak pertama yang menolak ide cacing gigi tersebut. Ia menyebutkan bahwa konsumsi gula-lah yang menjadi penyebab karies gigi.[17] Pada 1850, prevalensi karies meningkat lagi dan disebabkan oleh pergeseran pola makan.[3]
Pada 1890-an, W.D. Miller memulai rangkaian penelitian untuk menyelediki perihal penyakit karies gigi. Ia menemukan bahwa ada bakteri yang hidup di rongga mulut dan mengeluarkan asam sehingga melarutkan struktur gigi ketika terdapat sisi karbohidrat.[18] Penjelasan ini dikenal sebagai teori karies kemoparasitik.[19] Penemuan Miller, bersamaan penelitian terhadap plak gigi oleh G.V. Black dan J.L. Williams, membuat sebuah dasar sebagai penjelasan patofisiologi karies yang diterima hingga kini.[3]
Epidemiologi
Diperkirakan bahwa 90% dari anak-anak usia sekolah di seluruh dunia dan sebagian besar orang dewasa pernah menderita karies. Prevalensi karies tertinggi terdapat di Asia dan Amerika Latin. Prevalensi terendah terdapat di Afrika.[20] Di Amerika Serikat, karies gigi merupakan penyakit kronis anak-anak yang sering terjadi dan tingkatnya 5 kali lebih tinggi dari asma.[21] Karies merupakan penyebab patologi primer atas penanggalan gigi pada anak-anak.[22] Antara 29% hingga 59% orang dewasa dengan usia lebih dari limapuluh tahun mengalami karies.[23]
Jumlah kasus karies menurun di berbagai negara berkembang, karena adanya peningkatan kesadaran atas kesehatan gigi dan tindakan pencegahan dengan terapi florida.[24]
Classification
Caries can be classified by location, etiology, rate of progression, and affected hard tissues.[4] When used to characterize a particular case of tooth decay, these descriptions more accurately represent the condition to others and may also indicate the severity of tooth destruction.
Location
Generally, there are two types of caries when separated by location: caries found on smooth surfaces and caries found in pits and fissures.[25] The location, development, and progression of smooth-surface caries differ from those of pit and fissure caries.

Pit and fissure caries
Pits and fissures are anatomic landmarks on a tooth where tooth enamel infolds creating such an appearance. Fissures are formed during the development of grooves, and have not fully fused (unlike grooves), thus possessing a unique linear-like small depression in enamel's surface structure, which would be a great place for dental caries to develop and flourish. Fissures are mostly located on the occlusal (chewing) surfaces of posterior teeth and palatal surfaces of maxillary anterior teeth. Pits are small, pinpoint depressions that are found at the ends or cross-sections of grooves.[26] In particular, buccal pits are found on the facial surface of molars. For all types of pits and fissures, the deep infolding of enamel makes oral hygiene along these surfaces difficult, allowing dental caries to be common in these areas.
The occlusal surfaces of teeth represent 12.5% of all tooth surfaces but are the location of over 50% of all dental caries.[27] Among children, pit and fissure caries represent 90% of all dental caries.[28] Pit and fissure caries can sometimes be difficult to detect. As the decay progresses, caries in enamel nearest the surface of the tooth spreads gradually deeper. Once the caries reaches the dentin at the dentino-enamel junction, the decay quickly spreads laterally. Within the dentin, the decay follows a triangle pattern that points to the tooth's pulp. This pattern of decay is typically described as two triangles (one triangle in enamel, and another in dentin) with their bases conjoined to each other at the dentino-enamel junction (DEJ). This base-to-base pattern is typical of pit and fissure caries, unlike smooth-surface caries (where base and apex of the two triangles join).
Smooth-surface caries
There are three types of smooth-surface caries. Proximal caries, also called interproximal caries, form on the smooth surfaces between adjacent teeth. Root caries form on the root surfaces of teeth. The third type of smooth-surface caries occur on any other smooth tooth surface.

Proximal caries are the most difficult type to detect.[29] Frequently, this type of caries cannot be detected visually or manually with a dental explorer. Proximal caries form cervically (toward the roots of a tooth) just under the contact between two teeth. As a result, radiographs are needed for early discovery of proximal caries.[30]
Root caries, which are sometimes described as a category of smooth-surfaces caries, are the third most common type of caries and usually occur when the root surfaces have been exposed due to gingival recession. When the gingiva is healthy, root caries is unlikely to develop because the root surfaces are not as accessible to bacterial plaque. The root surface is more vulnerable to the demineralization process than enamel because cementum begins to demineralize at 6.7 pH, which is higher than enamel's critical pH.[31] Regardless, it is easier to arrest the progression of root caries than enamel caries because roots have a greater reuptake of fluoride than enamel. Root caries are most likely to be found on facial surfaces, then interproximal surfaces, then lingual surfaces. Mandibular molars are the most common location to find root caries, followed by mandibular premolars, maxillary anteriors, maxillary posteriors, and mandibular anteriors.
Lesions on other smooth surfaces of teeth are also possible. Since these occur in all smooth surface areas of enamel except for interproximal areas, these types of caries are easily detected and are associated with high levels of plaque and diets promoting caries formation.[29]
Other general descriptions
Besides the two previously mentioned categories, carious lesions can be described further by their location on a particular surface of a tooth. Caries on a tooth's surface that are nearest the cheeks or lips are called "facial caries", and caries on surfaces facing the tongue are known as "lingual caries". Facial caries can be subdivided into buccal (when found on the surfaces of posterior teeth nearest the cheeks) and labial (when found on the surfaces of anterior teeth nearest the lips). Lingual caries can also be described as palatal when found on the lingual surfaces of maxillary teeth because they are located beside the hard palate.
Caries near a tooth's cervix—the location where the crown of a tooth and its roots meet—are referred to as cervical caries. Occlusal caries are found on the chewing surfaces of posterior teeth. Incisal caries are caries found on the chewing surfaces of anterior teeth. Caries can also be described as "mesial" or "distal." Mesial signifies a location on a tooth closer to the median line of the face, which is located on a vertical axis between the eyes, down the nose, and between the contact of the central incisors. Locations on a tooth further away from the median line are described as distal.
Etiology

In some instances, caries are described in other ways that might indicate the cause. "Baby bottle caries", "early childhood caries", or "baby bottle tooth decay" is a pattern of decay found in young children with their deciduous (baby) teeth. The teeth most likely affected are the maxillary anterior teeth, but all teeth can be affected.[32] The name for this type of caries comes from the fact that the decay usually is a result of allowing children to fall asleep with sweetened liquids in their bottles or feeding children sweetened liquids multiple times during the day. Another pattern of decay is "rampant caries", which signifies advanced or severe decay on multiple surfaces of many teeth.[33] Rampant caries may be seen in individuals with xerostomia, poor oral hygiene, methamphetamine use (due to drug-induced dry mouth[34]), and/or large sugar intake. If rampant caries is a result from previous radiation to the head and neck, it may be described as radiation-induced caries. Problems can also be caused by the self destruction of roots and whole Tooth Resorption when new teeth erupt or later from unknown causes.
Rate of progression
Temporal descriptions can be applied to caries to indicate the progression rate and previous history. "Acute" signifies a quickly developing condition, whereas "chronic" describes a condition which has taken an extended time to develop. Recurrent caries, also described as secondary, is caries that appears at a location with a previous history of caries. This is frequently found on the margins of fillings and other dental restorations. On the other hand, incipient caries describes decay at a location that has not experienced previous decay. Arrested caries describes a lesion on a tooth which was previously demineralized but was remineralized before causing a cavitation.
Affected hard tissue
Depending on which hard tissues are affected, it is possible to describe caries as involving enamel, dentin, or cementum. Early in its development, caries may affect only enamel. Once the extent of decay reaches the deeper layer of dentin, "dentinal caries" is used. Since cementum is the hard tissue that covers the roots of teeth, it is not often affected by decay unless the roots of teeth are exposed to the mouth. Although the term "cementum caries" may be used to describe the decay on roots of teeth, very rarely does caries affect the cementum alone. Roots have a very thin layer of cementum over a large layer of dentin, and thus most caries affecting cementum also affects dentin.
Signs and symptoms

Until caries progresses, a person may not be aware of it.[35] The earliest sign of a new carious lesion, referred as incipient decay, is the appearance of a chalky white spot on the surface of the tooth, indicating an area of demineralization of enamel. As the lesion continues to demineralize, it can turn brown but will eventually turn into a cavitation, a "cavity". The process before this point is reversible, but once a cavitation forms, the lost tooth structure cannot be regenerated. A lesion which appears brown and shiny suggests dental caries was once present but the demineralization process has stopped, leaving a stain. A brown spot which is dull in appearance is probably a sign of active caries.
As the enamel and dentin are destroyed further, the cavitation becomes more noticeable. The affected areas of the tooth change color and become soft to the touch. Once the decay passes through enamel, the dentinal tubules, which have passages to the nerve of the tooth, become exposed and cause the tooth to hurt. The pain can be worsened by heat, cold, or sweet foods and drinks.[1] Dental caries can also cause bad breath and foul tastes.[36] In highly progressed cases, infection can spread from the tooth to the surrounding soft tissues which may become life-threatening, as in the case with Ludwig's angina.[37]
Diagnosis

Primary diagnosis involves inspection of all visible tooth surfaces using a good light source, dental mirror and explorer. Dental radiographs, produced when X-rays are passed through the jaw and picked up on film or digital sensor, may show dental caries before it is otherwise visible, particularly in the case of caries on interproximal (between the teeth) surfaces. Large dental caries are often apparent to the naked eye, but smaller lesions can be difficult to identify. Unextensive dental caries was formerly found by searching for soft areas of tooth structure with a dental explorer. Visual and tactile inspection along with radiographs are still employed frequently among dentists, particularly for pit and fissure caries.[38]
Some dental researchers have cautioned against the use of dental explorers to find caries.[29] In cases where a small area of tooth has begun demineralizing but has not yet cavitated, the pressure from the dental explorer could cause a cavitation. Since the carious process is reversible before a cavitation is present, it may be possible to arrest the caries with fluoride to remineralize the tooth surface. When a cavitation is present, a restoration will be needed to replace the lost tooth structure. A common technique used for the diagnosis of early (uncavitated) caries is the use of air blown across the suspect surface, which removes moisture, changing the optical properties of the unmineralized enamel. This produces a white 'halo' effect detectable to the naked eye. Fiberoptic transillumination, lasers and disclosing dyes have been recommended for use as an adjunct when diagnosing smaller carious lesions in pits and fissures of teeth.
Causes
There are four main criteria required for caries formation: a tooth surface (enamel or dentin); cariogenic (or potentially caries-causing) bacteria; fermentable carbohydrates (such as sucrose); and time.[39] The caries process does not have an inevitable outcome, and different individuals will be susceptible to different degrees depending on the shape of their teeth, oral hygiene habits, and the buffering capacity of their saliva. Dental caries can occur on any surface of a tooth that is exposed to the oral cavity, but not the structures which are retained within the bone.[40]
Teeth
There are certain diseases and disorders affecting teeth which may leave an individual at a greater risk for caries. Amelogenesis imperfecta, which occurs between 1 in 718 and 1 in 14,000 individuals, is a disease in which the enamel does not form fully or in insufficient amounts and can fall off a tooth.[41] Dentinogenesis imperfecta is a similar disease. In both cases, teeth may be left more vulnerable to decay because the enamel is not as able to protect the tooth as it would in health.[42]
In most people, disorders or diseases affecting teeth are not the primary cause of dental caries. Ninety-six percent of tooth enamel is composed of minerals.[43] These minerals, especially hydroxyapatite, will become soluble when exposed to acidic environments. Enamel begins to demineralize at a pH of 5.5.[44] Dentin and cementum are more susceptible to caries than enamel because they have lower mineral content.[45] Thus, when root surfaces of teeth are exposed from gingival recession or periodontal disease, caries can develop more readily. Even in a healthy oral environment, the tooth is susceptible to dental caries.
The anatomy of teeth may affect the likelihood of caries formation. In cases where the deep grooves of teeth are more numerous and exaggerated, pit and fissure caries are more likely to develop. Also, caries are more likely to develop when food is trapped between teeth.
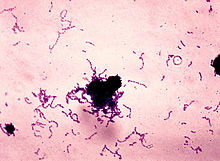
Bacteria
The mouth contains a wide variety of bacteria, but only a few specific species of bacteria are believed to cause dental caries: Streptococcus mutans and Lactobacilli among them.[5][7] Particularly for root caries, the most closely associated bacteria frequently identified are Lactobacillus acidophilus, Actinomyces viscosus, Nocardia spp., and Streptococcus mutans. Bacteria collect around the teeth and gums in a sticky, creamy-coloured mass called plaque, which serves as a biofilm. Some sites collect plaque more commonly than others. The grooves on the biting surfaces of molar and premolar teeth provide microscopic retention, as does the point of contact between teeth. Plaque may also collect along the gingiva. In addition, the edges of fillings or crowns can provide protection for bacteria, as can intraoral appliances such as orthodontic braces or removable partial dentures.
Fermentable carbohydrates
Bacteria in a person's mouth convert sugars (glucose and fructose, and most commonly sucrose - or table sugar) into acids such as lactic acid through a glycolytic process called fermentation.[6] If left in contact with the tooth, these acids may cause demineralization, which is the dissolution of its mineral content. The process is dynamic, however, as remineralization can also occur if the acid is neutralized; suitable minerals are available in the mouth from saliva and also from preventative aids such as fluoride toothpaste, dental varnish or mouthwash.[46] Caries advance may be arrested at this stage. If sufficient acid is produced over a period of time to the favor of demineralization, caries will progress and may then result in so much mineral content being lost that the soft organic material left behind would disintegrate, forming a cavity or hole.
Time
The frequency of which teeth are exposed to cariogenic (acidic) environments affects the likelihood of caries development.[47] After meals or snacks containing sugars, the bacteria in the mouth metabolize them resulting in acids as by-products which decreases pH. As time progresses, the pH returns to normal due to the buffering capacity of saliva and the dissolved mineral content from tooth surfaces. During every exposure to the acidic environment, portions of the inorganic mineral content at the surface of teeth dissolves and can remain dissolved for 2 hours.[48] Since teeth are vulnerable during these periods of acidic environments, the development of dental caries relies greatly on the frequency of these occurrences. For example, when sugars are eaten continuously throughout the day, the tooth is more vulnerable to caries for a longer period of time, and caries are more likely to develop than if teeth are exposed less frequently to these environments and proper oral hygiene is maintained. This is because the pH never returns to normal levels, thus the tooth surfaces cannot remineralize, or regain lost mineral content.
The carious process can begin within days of a tooth erupting into the mouth if the diet is sufficiently rich in suitable carbohydrates, but may begin at any other time thereafter. The speed of the process is dependent on the interplay of the various factors described above but is believed to be slower since the introduction of fluoride.[49] Compared to coronal smooth surface caries, proximal caries progress quicker and take an average of 4 years to pass through enamel in permanent teeth. Because the cementum enveloping the root surface is not nearly as durable as the enamel encasing the crown, root caries tends to progress much more rapidly than decay on other surfaces. The progression and loss of mineralization on the root surface is 2.5 times faster than caries in enamel. In very severe cases where oral hygiene is very poor and where the diet is very rich in fermentable carbohydrates, caries may cause cavitation within months of tooth eruption. This can occur, for example, when children continuously drink sugary drinks from baby bottles. On the other hand, it may take years before the process results in a cavity being formed, if at all.
Other risk factors
In addition to the four main requirements for caries formation, reduced saliva is also associated with increased caries rate since the buffering capability of saliva is not present to counterbalance the acidic environment created by certain foods. As a result, medical conditions that reduce the amount of saliva produced by salivary glands, particularly the parotid gland, are likely to cause widespread tooth decay. Some examples include Sjögren's syndrome, diabetes mellitus, diabetes insipidus, and sarcoidosis.[50] Medications, such as antihistamines and antidepressants, can also impair salivary flow.[51] Moreover, 63% of the most commonly prescribed medications in the United States list dry mouth as a known side effect.[50] Radiation therapy to the head and neck may also damage the cells in salivary glands, increasing the likelihood for caries formation.[52]
The use of tobacco may also increase the risk for caries formation. Smokeless tobacco frequently contains high sugar content in some brands, possibly increasing the susceptibility to caries.[53] Tobacco use is a significant risk factor for periodontal disease, which can allow the gingiva to recede.[54] As the gingiva loses attachment to the teeth, the root surface becomes more visible in the mouth. If this occurs, root caries is a concern since the cementum covering the roots of teeth is more easily demineralized by acids in comparison to enamel.[31] Currently, there is not enough evidence to support a causal relationship between smoking and coronal caries, but there is suggestive evidence of a causal relationship between smoking and root-surface caries.[55]
Pathophysiology

Enamel
Enamel is a highly mineralized acellular tissue, and caries act upon it through a chemical process brought on by the acidic environment produced by bacteria. The effects of this process include the demineralization of crystals in the enamel, caused by acids, over time until the bacteria physically penetrate the dentin. Enamel rods, which are the basic unit of the enamel structure, run perpendicularly from the surface of the tooth to the dentin. Since demineralization of enamel by caries generally follows the direction of the enamel rods, the different triangular patterns between pit and fissure and smooth-surface caries develop in the enamel because the orientation of enamel rods are different in the two areas of the tooth .[56]
As the enamel loses minerals , and dental caries progress, they develop several distinct zones, visible under a light microscope. From the deepest layer of the enamel to the enamel surface, the identified areas are the: translucent zone, dark zones, body of the lesion, and surface zone.[57] The translucent zone is the first visible sign of caries and coincides with a 1-2% loss of minerals.[58] A slight remineralization of enamel occurs in the dark zone, which serves as an example of how the development of dental caries is an active process with alternating changes.[59] The area of greatest demineralization and destruction is in the body of the lesion itself. The surface zone remains relatively mineralized and is present until the loss of tooth structure results in a cavitation.
Dentin
Unlike enamel, the dentin reacts to the progression of dental caries. After tooth formation, the ameloblasts, which produce enamel, are destroyed once enamel formation is complete and thus cannot later regenerate enamel after its destruction. On the other hand, dentin is produced continuously throughout life by odontoblasts, which reside at the border between the pulp and dentin. Since odontoblasts are present, a stimulus, such as caries, can trigger a biologic response. These defense mechanisms include the formation of sclerotic and tertiary dentin.[60]
In dentin from the deepest layer to the enamel, the distinct areas affected by caries are the translucent zone, the zone of bacterial penetration, and the zone of destruction.[56] The translucent zone represents the advancing front of the carious process and is where the initial demineralization begins. The zones of bacterial penetration and destruction are the locations of invading bacteria and ultimately the decomposition of dentin.

Sclerotic dentin
The structure of dentin is an arrangement of microscopic channels, called dentinal tubules, which radiate outward from the pulp chamber to the exterior cementum or enamel border.[61] The diameter of the dentinal tubules is largest near the pulp (about 2.5 μm) and smallest (about 900 nm) at the junction of dentin and enamel.[62] The carious process continues through the dentinal tubules, which are responsible for the triangular patterns resulting from the progression of caries deep into the tooth. The tubules also allow caries to progress faster.
In response, the fluid inside the tubules bring immunoglobulins from the immune system to fight the bacterial infection. At the same time, there is an increase of mineralization of the surrounding tubules.[63] This results in a constriction of the tubules, which is an attempt to slow the bacterial progression. In addition, as the acid from the bacteria demineralizes the hydroxyapatite crystals, calcium and phosphorus are released, allowing for the precipitation of more crystals which fall deeper into the dentinal tubule. These crystals form a barrier and slow the advancement of caries. After these protective responses, the dentin is considered sclerotic.
Fluids within dentinal tubules are believed to be the mechanism by which pain receptors are triggered within the pulp of the tooth.[64] Since sclerotic dentin prevents the passage of such fluids, pain that would otherwise serve as a warning of the invading bacteria may not develop at first. Consequently, dental caries may progress for a long period of time without any sensitivity of the tooth, allowing for greater loss of tooth structure.
Tertiary dentin
In response to dental caries, there may the production of more dentin toward the direction of the pulp. This new dentin is referred to as tertiary dentin.[62] Tertiary dentin is produced to protect the pulp for as long as possible from the advancing bacteria. As more tertiary dentin is produced, the size of the pulp decreases. This type of dentin has been subdivided according to the presence or absence of the original odontoblasts.[65] If the odontoblasts survive long enough to react to the dental caries, then the dentin produced is called "reactionary" dentin. If the odontoblasts are killed, the dentin produced is called "reparative" dentin.
In the case of reparative dentin, other cells are needed to assume the role of the destroyed odontoblasts. Growth factors, especially TGF-β,[65] are thought to initiate the production of reparative dentin by fibroblasts and mesenchymal cells of the pulp.[66] Reparative dentin is produced at an average of 1.5 μm/day, but can be increased to 3.5 μm/day. The resulting dentin contains irregularly-shaped dentinal tubules which may not line up with existing dentinal tubules. This dimishes the ability for dental caries to progress within the dentinal tubules.
Treatment

Destroyed tooth structure does not fully regenerate, although remineralization of very small carious lesions may occur if dental hygiene is kept at optimal level.[1] For the small lesions, topical fluoride is sometimes used to encourage remineralization. For larger lesions, the progression of dental caries can be stopped by treatment. The goal of treatment is to preserve tooth structures and prevent further destruction of the tooth.
Generally, early treatment is less painful and less expensive than treatment of extensive decay. Anesthetics — local, nitrous oxide ("laughing gas"), or other prescription medications — may be required in some cases to relieve pain during or following treatment or to relieve anxiety during treatment.[67] A dental handpiece ("drill") is used to remove large portions of decayed material from a tooth. A spoon is a dental instrument used to remove decay carefully and is sometimes employed when the decay in dentin reaches near the pulp.[68] Once the decay is removed, the missing tooth structure requires a dental restoration of some sort to return the tooth to functionality and aesthetic condition.
Restorative materials include dental amalgam, composite resin, porcelain, and gold.[69] Composite resin and porcelain can be made to match the color of a patient's natural teeth and are thus used more frequently when aesthetics are a concern. Composite restorations are not as strong as dental amalgam and gold; some dentists consider the latter as the only advisable restoration for posterior areas where chewing forces are great.[70] When the decay is too extensive, there may not be enough tooth structure remaining to allow a restorative material to be placed within the tooth. Thus, a crown may be needed. This restoration appears similar to a cap and is fitted over the remainder of the natural crown of the tooth. Crowns are often made of gold, porcelain, or porcelain fused to metal.

In certain cases, root canal therapy may be necessary for the restoration of a tooth.[71] Root canal therapy, also called "endodontic therapy", is recommended if the pulp in a tooth dies from infection by decay-causing bacteria or from trauma. During a root canal, the pulp of the tooth, including the nerve and vascular tissues, is removed along with decayed portions of the tooth. The canals are instrumented with endodontic files to clean and shape them, and they are then usually filled with a rubber-like material called gutta percha.[72] The tooth is filled and a crown can be placed. Upon completion of a root canal, the tooth is now non-vital, as it is devoid of any living tissue.
An extraction can also serve as treatment for dental caries. The removal of the decayed tooth is performed if the tooth is too far destroyed from the decay process to effectively restore the tooth. Extractions are sometimes considered if the tooth lacks an opposing tooth or will probably cause further problems in the future, as may be the case for wisdom teeth.[73] Extractions may also be preferred by patients unable or unwilling to undergo the expense or difficulties in restoring the tooth.
Prevention

Oral hygiene
Personal hygiene care consists of proper brushing and flossing daily.[8] The purpose of oral hygiene is to minimize any etiologic agents of disease in the mouth. The primary focus of brushing and flossing is to remove and prevent the formation of plaque. Plaque consists mostly of bacteria.[74] As the amount of bacterial plaque increases, the tooth is more vulnerable to dental caries. A toothbrush can be used to remove plaque on most surfaces of the teeth except for areas between teeth. When used correctly, dental floss removes plaque from areas which could otherwise develop proximal caries. Other adjunct hygiene aids include interdental brushes, water picks, and mouthwashes.
Professional hygiene care consists of regular dental examinations and cleanings. Sometimes, complete plaque removal is difficult, and a dentist or dental hygienist may be needed. Along with oral hygiene, radiographs may be taken at dental visits to detect possible dental caries development in high risk areas of the mouth.
Dietary modification
For dental health, the frequency of sugar intake is more important than the amount of sugar consumed.[47] In the presence of sugar and other carbohydrates, bacteria in the mouth produce acids which can demineralize enamel, dentin, and cementum. The more frequently teeth are exposed to this environment, the more likely dental caries are to occur. Therefore, minimizing snacking is recommended, since snacking creates a continual supply of nutrition for acid-creating bacteria in the mouth. Also, chewy and sticky foods (such as dried fruit or candy) tend to adhere to teeth longer, and consequently are best eaten as part of a meal. Brushing the teeth after meals is recommended. For children, the American Dental Association and the European Academy of Paediatric Dentistry recommend limiting the frequency of consumption of drinks with sugar, and not giving baby bottles to infants during sleep.[75][76] Mothers are also recommended to avoid sharing utensils and cups with their infants to prevent transferring bacteria from the mother's mouth.[77]
It has been found that milk and certain kinds of cheese like cheddar can help counter tooth decay if eaten soon after the consumption of foods potentially harmful to teeth.[47] Also, chewing gum containing xylitol (wood sugar) is widely used to protect teeth in some countries, being especially popular in the Finnish candy industry.[78] Xylitol's effect on reducing plaque is probably due to bacteria's inability to utilize it like other sugars.[79] Chewing and stimulation of flavour receptors on the tongue are also known to increase the production and release of saliva, which contains natural buffers to prevent the lowering of pH in the mouth to the point where enamel may become demineralised.[80]

Other preventive measures
The use of dental sealants is a good means of prevention. Sealants are thin plastic-like coating applied to the chewing surfaces of the molars. This coating prevents the accumulation of plaque in the deep grooves and thus prevents the formation of pit and fissure caries, the most common form of dental caries. Sealants are usually applied on the teeth of children, shortly after the molars erupt. Older people may also benefit from the use of tooth sealants, but their dental history and likelihood of caries formation are usually taken into consideration.
Fluoride therapy is often recommended to protect against dental caries. It has been demonstrated that water fluoridation and fluoride supplements decrease the incidence of dental caries. Fluoride helps prevent decay of a tooth by binding to the hydroxyapatite crystals in enamel.[81] The incorporated fluoride makes enamel more resistant to demineralization and, thus, resistant to decay.[82] Topical fluoride is also recommended to protect the surface of the teeth. This may include a fluoride toothpaste or mouthwash. Many dentists include application of topical fluoride solutions as part of routine visits.
Furthermore, recent research shows that low intensity laser radiation of argon ion lasers may prevent the susceptibility for enamel caries and white spot lesions.[83] Also, as bacteria are a major factor contributing to poor oral health, there is currently research to find a vaccine for dental caries. As of 2004, such a vaccine has been successfully tested on non-human animals,[84] and is in clinical trials for humans as of May 2006.[85]
See also
Footnotes and sources
- ^ a b c Dental Cavities, MedlinePlus Medical Encyclopedia, page accessed August 14, 2006.
- ^ a b c d e Epidemiology of Dental Disease, hosted on the University of Illinois at Chicago website. Page accessed January 9, 2007.
- ^ a b c d e f g h Suddick, Richard P. and Norman O. Harris. "Historical Perspectives of Oral Biology: A Series". Critical Reviews in Oral Biology and Medicine, 1(2), pages 135-151, 1990.
- ^ a b Sonis, Stephen T. "Dental Secrets: Questions and Answers Reveal the Secrets to the Principles and Practice of Dentistry." 3rd edition. Hanley & Belfus, Inc., 2003, p. 130. ISBN 1-56053-573-3.
- ^ a b Hardie, J.M. (1982). The microbiology of dental caries. Dental Update, 9, 199-208.
- ^ a b Holloway, P.J. (1983). The role of sugar in the etiology of dental caries. Journal of Dentistry, 11, 189-213.
- ^ a b Rogers A H (editor). (2008). Molecular Oral Microbiology. Caister Academic Press. ISBN 978-1-904455-24-0 .
- ^ a b Oral Health Topics: Cleaning your teeth and gums. Hosted on the American Dental Association website. Page accessed August 15, 2006.
- ^ Richards, MP. "A brief review of the archaeological evidence for Palaeolithic and Neolithic subsistence." European Journal of Clinical Nutrition, 56. 2002.
- ^ Freeth, Chrissie. "Ancient history of trips to the dentist" British Archaeology, 43, April 1999. Page accessed January 11, 2007.
- ^ a b History of Dentistry: Ancient Origins, hosted on the American Dental Association website. Page accessed January 9, 2007.
- ^ Dig uncovers ancient roots of dentistry: Tooth drilling goes back 9,000 years in Pakistan, scientists say, hosted on the MSNBC website. Page accessed on January 10, 2007.
- ^ Touger-Decker, Riva and Cor van Loveren. Sugars and dental caries, The American Journal of Clinical Nutrition, 78, 2003, pages 881S–892S.
- ^ Anderson, T. "Dental treatment in Medieval England", British Dental Journal, 2004, 197, pages 419-425.
- ^ Elliott, Jane. Medieval teeth 'better than Baldrick's', hosted on the BBC news website. October 8, 2004. Page accessed January 11, 2007.
- ^ Gerabek, W.E. "The tooth-worm: historical aspects of a popular medical belief." Clinical Oral Investigations. March 1999, 3(1), pages 1-6. Abstract hosted on the PubMed here.
- ^ McCauley, H. Berton. Pierre Fauchard (1678-1761), hosted on the Pierre Fauchard Academy website. The excerpt comes from a speech given at a Maryland PFA Meeting on March 13, 2001. Page accessed January 17, 2007.
- ^ Kleinberg, I. "A mixed-bacteria ecological approach to understanding the role of the oral bacteria in dental caries causation: an alternative to Streptococcus mutans and the specific-plaque hypothesis." Critical Reviews in Oral Biology and Medicine, 13(2), pages 108-125, 2002.
- ^ Baehni, P.C. and B. Guggenheim. "Potential of Diagnostic Microbiology for Treatment and Prognosis of Dental Caries and Periodontal Disease". Critical Reviews in Oral Biology and Medicine, 7(3), page 262, 1996.
- ^ The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme, released by the World Health Organization. (File in pdf format.) Page accessed on August 15, 2006.
- ^ Healthy People: 2010. Html version hosted on Healthy People.gov website. Page accessed August 13, 2006.
- ^ Frequently Asked Questions, hosted on the American Dental Hygiene Association website. Page accessed August 15, 2006.
- ^ "Dental caries", from the Disease Control Priorities Project. Page accessed August 15, 2006.
- ^ World Health Organization website, "World Water Day 2001: Oral health", page 2, page accessed August 14, 2006.
- ^ Summit, James B., J. William Robbins, and Richard S. Schwartz. "Fundamentals of Operative Dentistry: A Contemporary Approach." 2nd edition. Carol Stream, Illinois, Quintessence Publishing Co, Inc, 2001, p. 30. ISBN 0-86715-382-2.
- ^ Ash & Nelson, "Wheeler's Dental Anatomy, Physiology, and Occlusion." 8th edition. Saunders, 2003, p. 13. ISBN 0-7216-9382-2.
- ^ Doniger, Sheri, B. "Sealed." Dental Economics, 2003. Page accessed August 13, 2006.
- ^ Oral Health Resources - Dental Caries Fact Sheet. Hosted on the Centers for Disease Control and Prevention website. Page accessed August 13, 2006.
- ^ a b c Summit, James B., J. William Robbins, and Richard S. Schwartz. "Fundamentals of Operative Dentistry: A Contemporary Approach." 2nd edition. Carol Stream, Illinois, Quintessence Publishing Co, Inc, 2001, p. 31. ISBN 0-86715-382-2. Kesalahan pengutipan: Tanda
<ref>tidak sah; nama "summit31" didefinisikan berulang dengan isi berbeda - ^ Heatlh Strategy Oral Health Toolkit, hosted by the New Zealand's Ministry of Health. Page accessed on August 15, 2006.
- ^ a b Banting, D.W. "The Diagnosis of Root Caries." Presentation to the National Institute of Health Consensus Development Conference on Diagnosis and Management of Dental Caries Throughout Life, in pdf format, hosted on the National Institute of Dental and Craniofacial Research. Page 19. Page accessed on August 15, 2006. Kesalahan pengutipan: Tanda
<ref>tidak sah; nama "banting19" didefinisikan berulang dengan isi berbeda - ^ ADA Early Childhood Tooth Decay (Baby Bottle Tooth Decay). Hosted on the American Dental Association website. Page accessed August 14, 2006.
- ^ Radiographic Classification of Caries. Hosted on the Ohio State University website. Page accessed August 14, 2006.
- ^ ADA Methamphetamine Use (METH MOUTH). Hosted on the American Dental Association website. Page accessed February 14, 2007.
- ^ Health Promotion Board: Dental Caries, affiliated with the Singapore government. Page accessed on August 14, 2006.
- ^ Tooth Decay, hosted on the New York University Medical Center website. Page accessed August 14, 2006.
- ^ Ludwig's Anigna, hosted on Medline Plus. Page accessed on August 14, 2006.
- ^ Rosenstiel, Stephen F. Clinical Diagnosis of Dental Caries: A North American Perspective. Maintained by the University of Michigan Dentistry Library, along with the National Institutes of Health, National Institute of Dental and Craniofacial Research. 2000. Page accessed August 13, 2006.
- ^ Soames, J.V. and Southam, J.C. (1993). Oral Pathology, second edition, chapter 2 - Dental Caries.
- ^ Kidd, E.A.M. and Smith, B.G.N. (1990). Pickard's Manual of Operative Dentistry, Sixth Edition. Chapter 1 - Why restore teeth?.
- ^ Neville, B.W., Douglas Damm, Carl Allen, Jerry Bouquot. "Oral & Maxillofacial Pathology." 2nd edition, 2002, page 89. ISBN 0-7216-9003-3.
- ^ Neville, B.W., Douglas Damm, Carl Allen, Jerry Bouquot. "Oral & Maxillofacial Pathology." 2nd edition, 2002, page 94. ISBN 0-7216-9003-3.
- ^ Cate, A.R. Ten. "Oral Histology: development, structure, and function." 5th edition, 1998, p. 1. ISBN 0-8151-2952-1.
- ^ Dawes, Colin. "What Is the Critical pH and Why Does a Tooth Dissolve in Acid?." Journal of the Canadian Dental Association. Volume 69, Number 11, pages 722 - 724. December 2003. Hosted online. Page accessed August 14, 2006.
- ^ Mellberg, J.R. (1986). Demineralization and remineralization of root surface caries. Gerodontology, 5, 25-31.
- ^ Silverstone, L.M. (1983). Remineralization and dental caries: new concepts. Dental Update, 10, 261-273.
- ^ a b c "Dental Health", hosted on the British Nutrition Foundation website, 2004. Page accessed August 13, 2006.
- ^ Dental Caries, hosted on the University of California Los Angeles School of Dentistry website. Page accessed August 14, 2006.
- ^ Summit, James B., J. William Robbins, and Richard S. Schwartz. "Fundamentals of Operative Dentistry: A Contemporary Approach." 2nd edition. Carol Stream, Illinois, Quintessence Publishing Co, Inc, 2001, p. 75. ISBN 0-86715-382-2.
- ^ a b Neville, B.W., Douglas Damm, Carl Allen, Jerry Bouquot. "Oral & Maxillofacial Pathology." 2nd edition, 2002, page 398. ISBN 0-7216-9003-3.
- ^ Oral Health Topics A-Z: Dry Mouth, hosted on the American Dental Association website. Page accessed January 8, 2007.
- ^ Oral Complications of Chemotherapy and Head/Neck Radiation, hosted on the National Cancer Institute website. Page accessed January 8, 2007.
- ^ Neville, B.W., Douglas Damm, Carl Allen, Jerry Bouquot. "Oral & Maxillofacial Pathology." 2nd edition, 2002, page 347. ISBN 0-7216-9003-3.
- ^ Tobacco Use Increases the Risk of Gum Disease, hosted on the American Academy of Periodontology. Page accessed on January 9, 2007.
- ^ Executive Summary of U.S. Surgeon General's report titled, "The Health Consequences of Smoking: A Report of the Surgeon General," hosted on the CDC website, page 12. Page accessed January 9, 2007.
- ^ a b Kidd, E.A.M. and O. Fejerskov. "What Constitutes Dental Caries? Histopathology of Carious Enamel and Dentin Related to the Action of Cariogenic Biofilms," Journal of Dental Research, 83(Spec Iss C):C35-C38, 2004.
- ^ Darling, A.I. "Resistance of the Enamel to Dental Caries," Journal of Dental Research, 42(1): 488-496, 1963.
- ^ Robinson, C., R.C. Shore, S.J. Brookes, S. Strafford, S.R. Wood, and J. Kirkham. "The Chemistry of Enamel Caries," Critical Reviews in Oral Biology & Medicine, 11(4):481-495, 2000.
- ^ Cate, A.R. Ten. "Oral Histology: development, structure, and function." 5th edition, 1998, p. 417. ISBN 0-8151-2952-1.
- ^ "Teeth & Jaws: Caries, Pulp, & Periapical Conditions," hosted on the University of Southern California School of Dentistry website. Page accessed June 22, 2007.
- ^ Ross, Michael H., Gordon I. Kaye, and Wojciech Pawlina, 2003. Histology: a text and atlas. 4th edition. Page 450. ISBN 0-683-30242-6.
- ^ a b Cate, A.R. Ten. "Oral Histology: development, structure, and function." 5th edition, 1998, p. 152. ISBN 0-8151-2952-1.
- ^ Summit, James B., J. William Robbins, and Richard S. Schwartz. "Fundamentals of Operative Dentistry: A Contemporary Approach." 2nd edition. Carol Stream, Illinois, Quintessence Publishing Co, Inc, 2001, p. 13. ISBN 0-86715-382-2.
- ^ Dababneh, R.H., A.T. Khouri and M. Addy. "Dentine hypersensitivity - an enigma? a review of terminology, mechanisms, aetiology and management." British Dental Journal, vol. 187, no. 11, December 11, 1999. Page accessed June 22, 2007. The referred to theory is the widely-accepted hydrodynamic theory of sensitivity.
- ^ a b Smith, A.J., P.E. Murray, A.J. Sloan, J.B. Matthews, S. Zhao. "Trans-dentinal Stimulation of Tertiary Dentinogenesis," Advances in Dental Research, 15, pp. 51 -54, August, 2001. Page accessed June 23, 2007.
- ^ Summit, James B., J. William Robbins, and Richard S. Schwartz. "Fundamentals of Operative Dentistry: A Contemporary Approach." 2nd edition. Carol Stream, Illinois, Quintessence Publishing Co, Inc, 2001, p. 14. ISBN 0-86715-382-2.
- ^ Oral Health Topics: Anesthesia Frequently Asked Questions, hosted on the American Dental Association website. Page accessed August 16, 2006.
- ^ Summit, James B., J. William Robbins, and Richard S. Schwartz. "Fundamentals of Operative Dentistry: A Contemporary Approach." 2nd edition. Carol Stream, Illinois, Quintessence Publishing Co, Inc, 2001, p. 128. ISBN 0-86715-382-2.
- ^ "Aspects of Treatment of Cavities and of Caries Disease" from the Disease Control Priorities Project. Page accessed August 15, 2006.
- ^ Oral Health Topics: Dental Filling Options, hosted on the American Dental Association website. Page accessed August 16, 2006.
- ^ What is a Root Canal?, hosted by the Academy of General Dentistry. Page accessed on August 16, 2006.
- ^ FAQs About Root Canal Treatment, hosted on the American Association of Endodontists website. Page accessed August 16, 2006.
- ^ Wisdom Teeth, packet in pdf format hosted by the American Association of Oral and Maxillofacial Surgeons. Page accessed on August 16, 2006.
- ^ Introduction to Dental Plaque. Hosted on the Leeds Dental Institute Website, page accessed August 14, 2006.
- ^ A Guide to Oral Health to Prospective Mothers and their Infants, hosted on the European Academy of Paediatric Dentistry website. Page accessed August 14, 2006.
- ^ Oral Health Topics: Baby Bottle Tooth Decay, hosted on the American Dental Association website. Page accessed August 14, 2006.
- ^ Guideline on Infant Oral Health Care, hosted on the American Academy of Pediatric Dentistry website. Page accessed January 13, 2007.
- ^ "History", hosted on the Xylitol.net website. Page accessed October 22, 2006.
- ^ Ly KA, Milgrom P, Roberts MC, Yamaguchi DK, Rothen M, Mueller G. Linear response of mutans streptococci to increasing frequency of xylitol chewing gum use: a randomized controlled trial. BMC Oral Health. 2006 Mar 24;6:6.
- ^ Bots CP, Brand HS, Veerman EC, van Amerongen BM, Nieuw Amerongen AV. Preferences and saliva stimulation of eight different chewing gums. Int Dent J. 2004 Jun;54(3):143-8.
- ^ Cate, A.R. Ten. "Oral Histology: development, structure, and function." 5th edition, 1998, p. 223. ISBN 0-8151-2952-1.
- ^ Ross, Michael H., Gordon I. Kaye, and Wojciech Pawlina, 2003. "Histology: a text and atlas." 4th edition, p. 453. ISBN 0-683-30242-6.
- ^ In vitro caries formation in primary tooth enamel: Role of argon laser irradiation and remineralizing solution treatment. Journal of the American Dental Association, Volume 137, Number 5, p. 638-644. Page accessed August 18, 2006.
- ^ New Drill for Tomorrow's Dentists. WIRED Magazine, May, 2004. Page accessed May 24, 2007.
- ^ "Planet Biotechnology:Products". Planet Biotechnology.
References
|
Printed sources
|
Online sources
|
External links
- What causes cavities; an indepth look
- Links to tooth decay pictures (Hardin MD/Univ of Iowa)
- Caries Diagnosis - Coronal Caries from the University of Michigan, School of Dentistry.
- Diet, Nutrition and the prevention of chronic diseases (including dental caries) by a Joint WHO/FAO Expert consultation (2003) .
- Image showing various stages of dental caries
- Global Oral Health - CaPP, a chart containing caries data from selected countries.
